During the transition to digital medicine, ethical issues have become key. They largely determine the speed of technological progress in this area.
Big data and AI technologies make it possible to raise disease diagnosis, treatment and prevention to a new level. However, there is an urgent question to what extent it is possible to use patient information on citizens' health for AI training: limited use slows down AI technology development, and unlimited use is fraught with discrimination and violation of individual rights and freedoms.
Today we will shine light on the topic of information governance, breaches of confidentiality and their consequences.
Stay tuned!
Learn how to simplify your practice workflow and free up more time for patients with Medesk.
Open the detailed description >>Personal Data in Health and Social Care
A person's medical condition and health are documented in various ways. Some of the data is actually produced as a result of personal care, and some of the data can be obtained in connection with these two processes. They have different legal status, different opportunities for third parties to access them, but both raise ethical questions.
Data sources in medicine in the broadest sense:
- Mobile applications for public health
- Sensors and monitoring devices
- Laboratory data, X-rays
- Data obtained in scientific research involving groups of patients
- Data on the purchase of medicines and other medical care products by patients
- Data from social networks, search queries, etc.
Biomedical data is information that constitutes a health privacy. This medical, legal, social and ethical concept prohibits a healthcare professional from informing third parties about the patient's care status. Medical privacy is one of the most important principles of professional health ethics. It is protected by the law.
In the digital age, medical documents and other information constituting a medical privacy are not the only sources of data on a person's physical condition and health. Social media, search query history, data on visits to clinical institutions, purchases also become sources of data that can be used when assessing risks in insurance or hiring. But such data is not covered by health privacy laws.
There is a problem of effective ethical circulation and use of medical data.
Medesk helps automate scheduling and record-keeping, allowing you to recreate an individual approach to each patient, providing them with maximum attention.
Learn more >>Big Data and Data-driven Technologies
Before using big data, we need to solve the main ethical question:
How to ensure private information confidentiality?
It is pertinent to note that big data does not require an unambiguous indication of belonging to a particular group. It allows you to identify its signs automatically (for example, taking certain medications may indicate HIV status). If the access to sensitive information about physical, mental health, suicidal tendencies is opened, this may lead to discrimination in hiring, inequality in health insurance, etc.
In the UK, after a long discussion, a Code of Conduct for Data-Driven Health and Care Technologies was formulated. According to the creators, this code should become part of the overall digital national strategy. It should help create an environment that supports innovative technologies using data, ensuring security, competitiveness, compliance with ethical and legal obligations.
The Code outlines standards for data protection, consent, data sharing, cybersecurity, and fair data use. It fosters a responsible and trustworthy environment for the development and deployment of data-driven health and care technologies.
Guide to Confidentiality in Health and Social Care
Patient confidentiality in the health and social care sectors is crucial for several reasons. Let’s discuss them in more detail, so you can make your private practice a place where your patients and members of staff feel safe and secure.
#1. Trust
Confidentiality is a fundamental aspect of building trust between healthcare providers, social care workers, and individuals receiving care. When people share sensitive information about their health, personal lives, or social circumstances, they expect it to be treated with the utmost privacy. Respecting confidentiality preserves dignity and autonomy.
If you break this trust, stable patient retention becomes impossible to achieve.
#2. Patient-centered care
By safeguarding confidentiality, healthcare professionals demonstrate their commitment to patient-centered care. When individuals have confidence that their personal information will remain confidential, they are more likely to disclose important details about their health. This enables accurate diagnoses and appropriate treatment plans.
#3. Legal requirements
Many countries have legal and ethical frameworks in healthcare and social care settings. These frameworks, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States or the General Data Protection Regulation (GDPR) in the European Union, are designed to protect individuals' privacy rights and ensure personal information security.
Moreover, there are several acts and laws that regulate doctor-patient relationships in data protection.
The Common Law of Confidentiality refers to the legal principles and rules developed through court decisions and judicial precedent to protect information confidentiality. Common law varies among jurisdictions, but there are several general principles commonly recognized:
Duty of сonfidentiality in certain relationships, such as doctor-patient, lawyer-client, therapist-patient, and priest-penitent.
Scope of сonfidentiality covers all information disclosed in confidence by the client or patient to the professional.
Exceptions to сonfidentiality include situations where there is a legal duty or risk of harm to disclose when required by court order.
Consent. If a person provides informed consent for their information to be shared with specific individuals or entities, the duty of confidentiality may no longer apply to that particular information.
The Care Act 2014 aims to reform and simplify the social care system. It aims to promote well-being, and ensure access to high-quality care and support.
According to the Act, local authorities must consider a person's well-being in all decision-making processes and focus on achieving desired outcomes that contribute to their well-being. This includes respecting patients’ preferences, choices, and privacy rights which involve confidentiality considerations.
Not to mention, the Act recognizes unpaid carers' rights and their entitlement to support. Confidentiality plays a role in the assessment and provision of support to caregivers, ensuring their information is treated with respect and privacy.
The Data Protection Act 2018 in the United Kingdom is comprehensive legislation that governs personal data processing and protection. While the DPA 2018 primarily focuses on data protection, it includes provisions relevant to confidentiality, as it is closely tied to personal information protection.
Discover more about the essential features of Medesk and claim your free access today!
Explore now >>The DPA 2018 imposes obligations on data controllers and processors to maintain personal data confidentiality. This includes implementing appropriate technical and organizational measures to protect against unauthorized access, disclosure, or loss of medical records.
The maximum fine that can be imposed for a data protection breach is £8.7 million or 2% of the total annual worldwide turnover , whichever is higher.
Such measures may include the use of encryption, and access controls. Moreover, data controllers and processors must ensure that all data is securely destroyed when it is no longer needed.
The Act also mandates that care providers implement appropriate technical and organizational measures to ensure information security.
#4. Psychological safety
Confidentiality promotes psychological safety for effective care of an individual and social service users. It encourages open communication and allows patients to share their concerns, fears, and sensitive information with care teams without judgment. This safe and trusting environment fosters strong therapeutic relationships and effective care services.
#5. Data security
Confidentiality measures also contribute to data security. In the age of electronic health records and digital information sharing, protecting data is essential. Maintaining confidentiality through secure systems, proper access controls, and encryption techniques prevents unauthorized access, identity theft, and breaches that could compromise personal information.
Protecting electronic health records from malware is essential, and solutions like Bitdefender antivirus free help safeguard sensitive patient data on Windows devices against cyber threats.
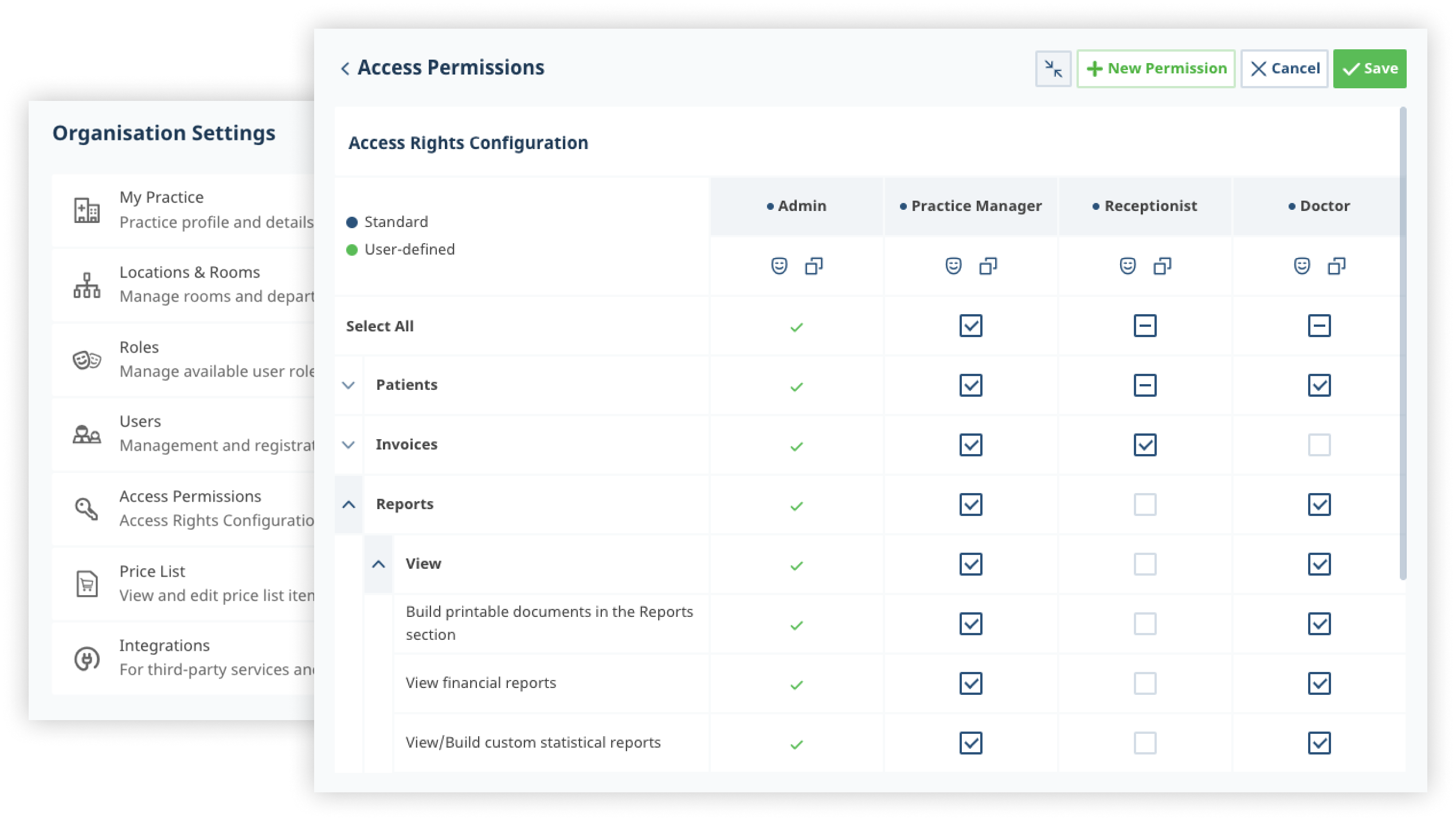
With practice management software all medical data you enter is protected and stored. Different levels of access rights help you to build trustworthy relationships with your staff and patients. All data is available 24/7 and can be deleted upon request at any time.
What if You Violate the Confidentiality Rules?
We are all humans after all. Sometimes health and social workers unwillingly break patient confidentiality. If it happens, be ready to deal with the consequences and apologize for the mistake.
What consequences can you expect if confidentiality is broken?
Legal consequences
Violating laws and regulations, such as HIPAA or the DPA can result in legal penalties, fines, or even criminal charges for the responsible party or organization. And of course, don’t forget about the loss of trust from your current and potential patients.
Professional consequences
They include disciplinary actions, loss of licensure, or damage to professional reputation. Breaching confidentiality is considered a serious ethical violation in these fields and can have severe professional ramifications.
Such breaches not only harm the affected individuals but also damage the credibility of the healthcare or social care organization responsible for safeguarding the information.
Emotional and psychological impact
Violations may lead to feelings of embarrassment, shame, or distress, particularly if the disclosed information is stigmatized. The person may also experience anxiety about his confidential information being further disclosed or used against him.
To prevent confidentiality breaches, healthcare and social care professionals must understand and follow confidentiality guidelines. They must maintain secure systems for data storage and transmission, and uphold ethical and legal standards to protect individuals' privacy.
To make this process easier to bear, utilize modern practice management software. We’ve got you covered here.
Provide your patients and colleagues with the protection they deserve.


