In the world of mental health documentation, clarity, structure, and comprehensiveness are essential. One of the most widely adopted methods for documenting clinical interactions is the DAP note.
This article explores what DAP notes are, who can use them, how to create them, provides examples in mental health contexts, and compares them with SOAP notes. Whether you're a seasoned professional or new to the field, this guide will provide valuable insights into the effective use of DAP notes.
What is a DAP Note?
It is an acronym. DAP stands for data, assessment, and plan. DAP progress notes are a method of documentation used by healthcare professionals, particularly in the mental health field, to record patient interactions, progress, and treatment plans.
Learn how to simplify your practice workflow and free up more time for patients with Medesk.
Open the detailed description >>The structure of DAP notes ensures that all relevant information is captured in a clear and organised manner.
Breakdown of DAP format:
- The data section includes factual information gathered during the session. It can encompass observations, direct quotes from the client, and objective details such as the client's appearance, mood, and behavior. The data should be precise and free of interpretation.
- In the assessment section, the clinician provides an analysis of the data. This section is more subjective, as it involves the clinician's professional judgement and insights. It includes interpretations of the client's condition, progress, and any issues identified during the session.
- The plan section outlines the next steps in the client's treatment. It includes the clinician's recommendations, goals for future sessions, and any planned interventions. The plan should be specific, actionable, and tailored to the client's needs.
Who Can Use DAP Notes?
DAP notes are used by a variety of healthcare professionals, particularly those in the mental health field. This includes:
- Psychologists use DAP notes to document therapy sessions, track patient progress, and develop treatment plans.
- Psychiatrists implement this note format to record patient interactions, medication management, and therapeutic interventions.
- Licensed Clinical Social Workers (LCSWs) document their client interactions and therapy sessions using DAP notes to ensure comprehensive care.
- Nurses and nurse practitioners. These healthcare providers use DAP note-taking to also document patient interactions and treatment plans.
How to Create DAP Notes
Creating effective DAP notes requires attention to detail and a structured approach. Here are the steps to create comprehensive DAP notes:
Step-by-Step Guide to Creating DAP Notes:
Start with data:
- Record what you observe during the session. This might include the client's appearance, behaviour, and any notable physical signs.
- Document significant quotes or statements made by the client. These should be verbatim to capture the client's perspective accurately.
- Note the time, date, and setting of the session. Include any other relevant details, such as the client's participation or engagement level.
Move to assessment:
- Analyse the data collected. Use your professional judgement to interpret the client's statements and behaviours.
- Assess the client's progress towards their treatment goals. Identify any new issues or challenges that have emerged.
- Include your clinical impressions or diagnoses based on the data. Be sure to support these with evidence from the session.
Conclude with the plan:
- Next Steps: Outline the immediate next steps for the client's treatment. This might include scheduling the next session, recommending specific interventions, or adjusting treatment plans.
- This section of a DAP note outlines goals for future sessions. These should be specific, measurable, achievable, relevant, and time-bound (SMART goals).
- Assign any tasks or responsibilities to the client, such as homework assignments or behaviour changes to focus on.
We advise to use technology to make the process easier and faster. For example, you can utilise EHR systems for efficient documentation and use voice-to-text technology to dictate notes immediately during and after sessions.
Medesk helps automate scheduling and record-keeping, allowing you to recreate an individual approach to each patient, providing them with maximum attention.
Learn more >>An Example of DAP Notes in Mental Health
To illustrate how DAP notes are used in practice, let's consider an example from a therapy session:
DAP Note Example Scenario:
Client: Jane Doe
Session Date: June 5, 2024
Therapist: Dr. John Smith, Psy.D.Data (D):
Jane appeared anxious, with rapid speech and fidgeting throughout the session.
She reported feeling overwhelmed at work and experiencing difficulty sleeping for the past two weeks.
Jane stated, "I can't shut my mind off at night. It's like I'm constantly thinking about work."
Assessment (A):
Jane's anxiety appears to be exacerbated by work-related stress.
Her difficulty sleeping is likely contributing to her overall sense of overwhelm and decreased ability to cope with stress.
There is a notable increase in her anxiety symptoms compared to the previous session, indicating a need for intervention to address sleep and stress management.
Plan (P):
Introduce cognitive-behavioural strategies to help Jane manage her anxiety and work-related stress.
Recommend practicing relaxation techniques before bedtime to improve sleep hygiene.
Schedule a follow-up session in one week to assess progress and adjust the treatment plan as necessary.
Assign Jane the task of keeping a sleep diary to monitor her sleep patterns and identify potential triggers for her insomnia.
Comparing DAP and SOAP Notes
While DAP notes are a valuable tool for many mental health professionals, they are not the only method of documentation.
Another widely used format is SOAP notes, which stands for subjective, objective, assessment, and plan. Understanding the differences between these two formats can help clinicians choose the best approach for their practice.
SOAP Notes Breakdown:
Subjective. This section includes the client's subjective experiences, symptoms, and feelings. It often incorporates the client's own words and descriptions of their condition.
Objective. This part contains observable data, such as the clinician's observations, physical examination findings, and any test results.
Assessment. Similar to the DAP notes, this section involves the clinician's interpretation of the subjective and objective data, including diagnoses and clinical impressions.
Plan. The plan section outlines the treatment strategy, including any interventions, follow-up plans, and patient instructions.
Key Differences Between DAP and SOAP Notes:
Structure and Focus:
DAP Notes: Emphasise a straightforward, three-part structure focused on data, assessment, and planning. This format is particularly useful for mental health professionals who need to capture both objective observations and subjective interpretations within a concise framework.
SOAP Notes: Provide a four-part structure that distinguishes between subjective and objective information. This can be advantageous in settings where differentiating between the patient's subjective experience and objective data is crucial, such as in medical or multidisciplinary contexts.
Flexibility:
DAP Notes: Offer more flexibility in combining subjective and objective data in the "Data" section, which can simplify documentation for certain mental health sessions.
SOAP Notes: Require a clear separation of subjective and objective information, which can be beneficial for creating a comprehensive and detailed record but may be more time-consuming.
Usage Context:
DAP Notes: Commonly used in mental health settings where the emphasis is on therapeutic progress, client engagement, and treatment planning.
SOAP Notes: Widely used across various healthcare settings, including primary care, nursing, and physical therapy, where detailed differentiation of subjective and objective data is necessary.
Use Our Pre-built DAP Note Template
Writing DAP notes is an easy and convenient way to record a client's progress during psychotherapy. No therapist knows how many sessions a client will need to improve their quality of life. Nor does he or she know how many times clinical notes will have to be filled out. Dozens? Hundreds of times?
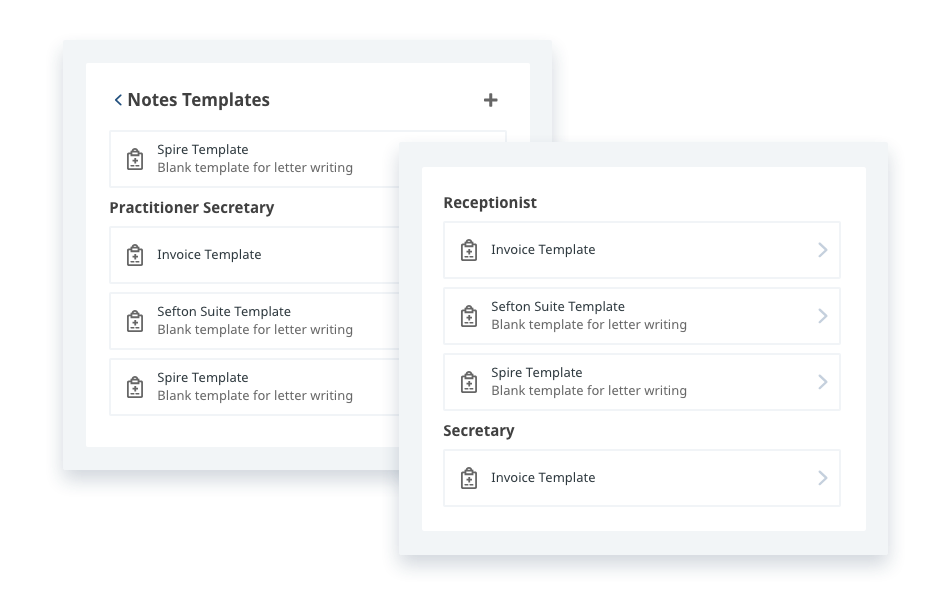
To optimise the time spent with the patient in a session, use practice management software with ready-made templates for the main types of therapy notes.
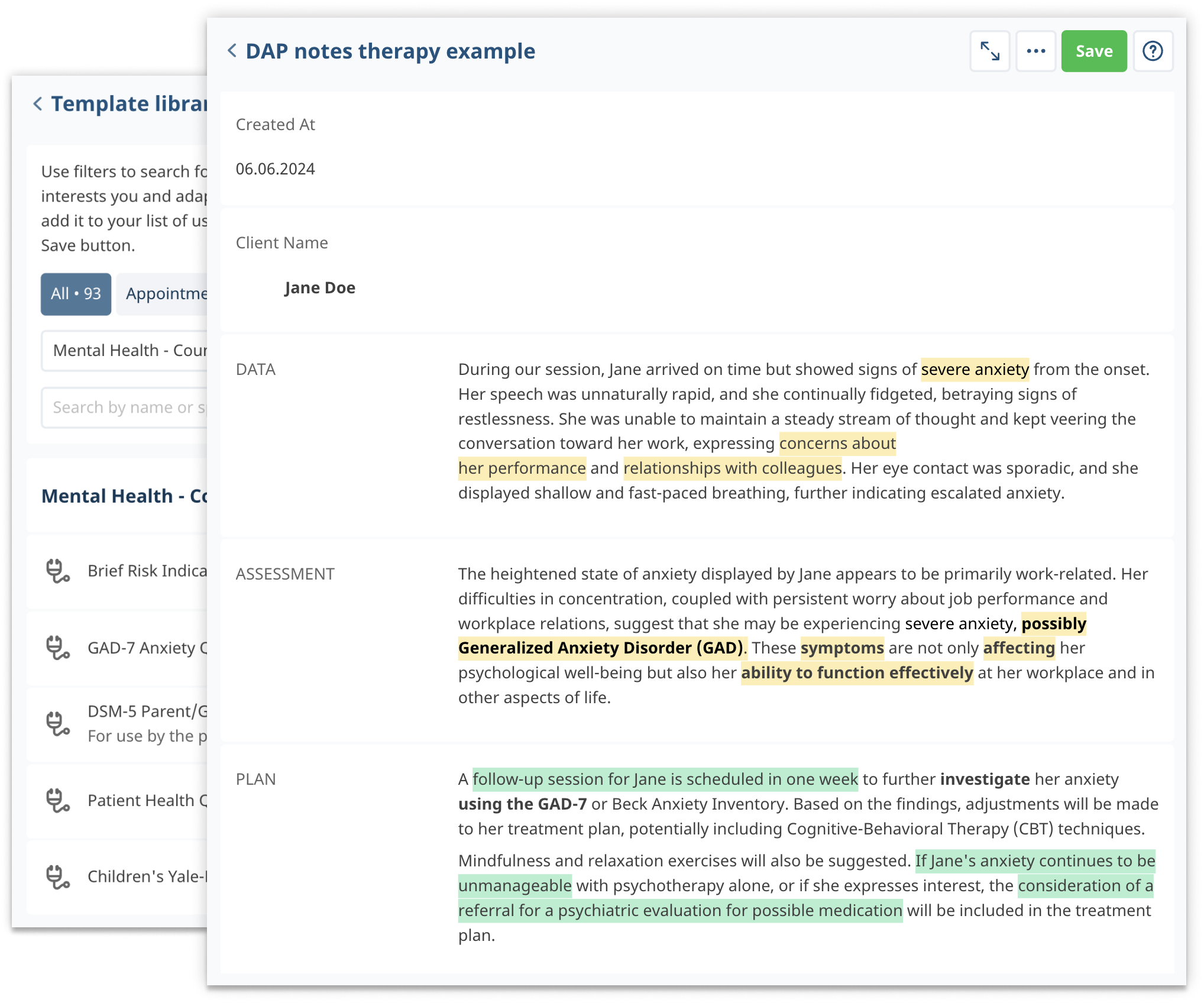
With our template library, not only can you quickly create different types of notes, but you can also create health packages and treatment plans, send online forms to patients, use the ICD-10 database, and create your own unique templates for your private practice.
Discover more about the essential features of Medesk and claim your free access today!
Explore now >>DAP notes are a valuable tool for mental health professionals, providing a structured yet flexible method for documenting client interactions, assessments, and treatment plans.
By understanding the components of DAP notes and how to create them effectively, you enhance your documentation practices, improve communication with colleagues, and ultimately provide better continuity of care for your clients.


