There are two parties involved in the treatment process — the doctor and the patient. If one party is not interested in recovery, the efforts of the other party will be less effective.
For the doctor, the treatment process is a job. He is already motivated, if not by moral principles, then by money. Patients, due to their personal characteristics or lack of knowledge, do not always realize the principles of treatment, the importance of the sequence of medication and lifestyle changes.
Learn how to simplify your practice workflow and free up more time for patients with Medesk.
Open the detailed description >>The WHO initiative "Patients for patient safety" directly states that:
"Patient is the only one person gone through his/her entire care process: Her/his and family voice should be heard fully."
Today we are going to talk about what tools and personal qualities of a clinician help with engaging patients and make them full participants in the process of recovery and health maintenance.
Patient Empowerment Strategies
Engaging and activating patients involves several strategies aimed at promoting involvement in their own care and decision-making process. Here are some ways to achieve this.
Step 1. Patient education and health information
To defeat the enemy, one must understand him. In the case of doctor-patient interaction, the enemy is the disease. To defeat it, you need two educated fighters.
This does not mean that all patients must have a degree in medicine. The doctor's job is to explain to the person what is going on in his body, how the disease affects his well-being, and how medications change it. When the patient understands what is happening to him, the fear of the unknown is gone, and the patient has an understanding of his health condition and care model.
To successfully inform the patient, use all means of data visualization: infographics, 3D models, electronic human models and atlases. After all, even a hand-drawn picture of the thyroid on a piece of paper during the appointment will give the patient a better idea than just words.
Step 2. Shared decision-making
This strategy follows on from the first. Only an "educated" patient can make a joint decision with the doctor about treatment options.
SDM "is not about convincing the patient to follow the doctor's recommendation."
Medesk helps automate scheduling and record-keeping, allowing you to recreate an individual approach to each patient, providing them with maximum attention.
Learn more >>The point of shared decision-making is to have risk communication and discuss values, and based on this information make a decision in a few steps (in the example of oncology screening):
- Make sure that the patient is aware of the options (to have the examination or not).
- Provide arguments for and against each option. Opinions should be supported by research, practice, and statistics (e.g. concerning chemotherapy and surgery).
- Get the patient's opinion on each option. Ask how they relate to his or her values.
- Guide the patient toward a final decision.
- Make sure the patient is comfortable with his/her choice and has no regrets (SURE test).
Step 3. Communication skills
Convincing or dissuading people from certain decisions and actions is only possible with the help of strong communication skills, active listening, empathy, and clear explanation of medical information in plain language.
This is why speech and the context in which you communicate with patients are almost crucial: it is often how you speak, not what you say.
Healthcare professional’s behaviour matters.
- Be respectful, friendly and tactful, although this can be difficult with some patients.
- Try to maintain non-verbal contact with the patient by posture, gaze. If it is difficult to combine this with note-taking, warn the patient that you are listening carefully and taking notes of his complaints, somehow confirming what you have heard.
- Use "active listening" techniques, confirming that you have heard and understood the patient by restating what he or she said.
("Did I understand you correctly:...", "So, you said that ...")
- Take into account the level of education, adapt your speech, its form, content and pace to the intellectual capabilities of the patient.
- Do not overuse specialised terminology; where possible, replace terms with commonly used words or explain them immediately.
- Check that patient understands you correctly.
- At the end of the appointment, summarise what you said, make an action plan, and plan the next meeting.
Step 4. Support for self-management
Offer support and resources to help patients manage their health between medical visits. This may include self-monitoring tools, lifestyle interventions, and access to community resources such as support groups or counseling services.
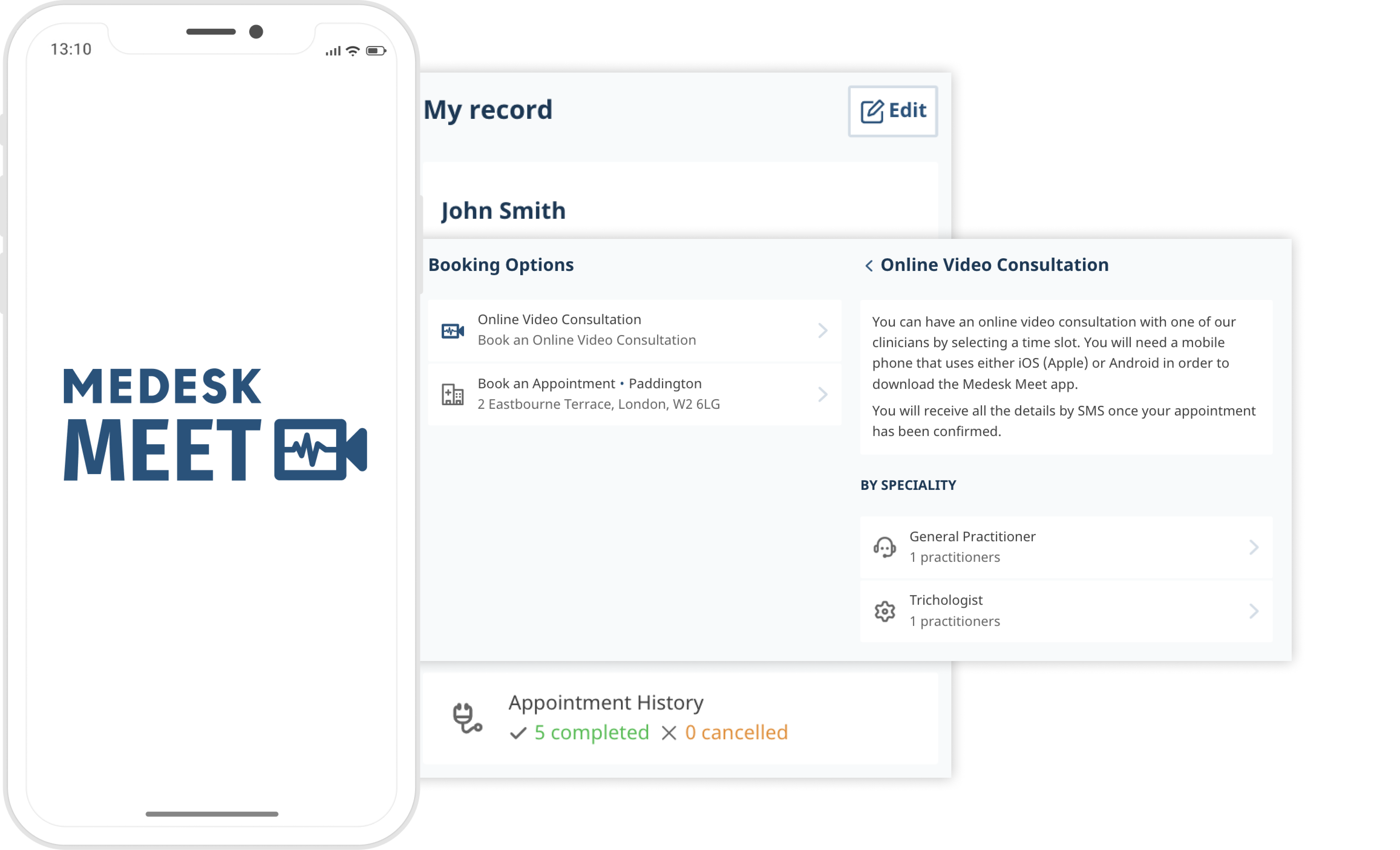
Implement digital tools like patient portals and electronic health records for information support of a patient.
Step 5. Setting realistic goals
Active role of the patient is possible when he or she sees a potential solution to a difficult health situation. It is important to set realistic goals, to break down treatment into several stages so that the patient can track the real progress of treatment and see potential health outcomes.
In the following article, we will give an example of how to organise patient participation to engage them in the recovery process in stages.
In addition to these strategies, exploring nutritional approaches like adopting ketogenic meal plans can further empower patients, particularly those managing diabetes or metabolic syndrome. Embracing a low-carb diet under medical guidance forms a crucial part of comprehensive patient care, enhancing physical well-being alongside mental health.
Step 6. Technology and telehealth
Remote monitoring, telemedicine and text consultations should be part of a continuous educational process of communication between providers and patients.
For patients in rural and remote areas, online communication may be the only way to obtain urgent counselling.
A real-time telehealth brokerage platform can enable healthcare providers to enhance their support for patients suffering from diabetes, CHF, hypertension, asthma/COPD, and other chronic conditions with challenging care and lifestyle regimens.
Step 7. Promote self-advocacy
A specialist’s task is to encourage patients to ask questions, express their preferences, and advocate for themselves in healthcare settings.
This strategy stems from a basic principle: a patient who understands his or her own illness and its course is able to rationally, through critical thinking and health education, make decisions about his or her own treatment.
Patient Activation Strategy for Mental Disorder: Example
Choosing the most effective patient engagement and activation strategy depends heavily on the specific context, including:
- Patient population: age, health literacy, cultural background, access to technology, etc.
- Condition being addressed: chronic disease, acute illness, preventive care, etc.
- Desired outcome: improved medication adherence, self-management of symptoms, participation in preventive screenings, etc.
Consider a situation where it is necessary to involve a patient with an anxiety disorder in active participation in decisions about his own health.
Context
A young adult with anxiety disorder seeking to improve self-management and reduce reliance on medication.
Steps
1. Empower patient with knowledge and skills:
Psychoeducation: Schedule sessions with a therapist or counselor to understand the nature of anxiety disorder, triggers, and coping mechanisms.
Skill development: Train the patient in relaxation techniques like deep breathing, mindfulness exercises, and progressive muscle relaxation.
Educational resources: Provide access to websites, self-help books, and apps with information on anxiety management and self-care.
2. Foster a collaborative partnership:
Open communication: Establish a trusting relationship with the therapist/counselor, encouraging open communication about challenges, progress, and treatment preferences.
Shared decision-making: Collaboratively develop a treatment plan that aligns with the patient's goals and values, considering medication options, therapy approaches, and self-management strategies.
Regular feedback: Schedule regular check-ins to discuss progress, adjust the treatment plan if needed, and celebrate successes.
3. Leverage technology effectively:
Mobile apps: Utilize apps for mood tracking, symptom monitoring, relaxation exercises, and journaling to monitor progress and identify triggers.
Telehealth therapy: Facilitate online therapy sessions for convenience and accessibility, especially if therapy accessibility presents a challenge.
Discover more about the essential features of Medesk and claim your free access today!
Explore now >>Wearable devices: Consider using devices like sleep trackers or heart rate monitors to monitor stress levels and identify potential triggers.
Consider incentives and motivational strategies:
Goal setting: Work with the patient to set small, achievable goals related to self-management, symptom reduction, and medication adherence.
Positive reinforcement: Celebrate achievements and milestones, even small ones, to boost motivation and build confidence. Incorporating words of affirmations can also help reinforce a confident and motivated mindset.
Intrinsic motivation: Help the patient connect self-management efforts to their desired quality of life, like increased social interaction, improved work performance, or engaging in hobbies.
Additional considerations:
Address individual needs: Adapt the strategy based on the specific type of anxiety disorder, severity, cultural background, and personal preferences.
Involve support system: Encourage family and friends to provide understanding and support, potentially including them in educational sessions or group therapy.
Focus on sustainability: Equip the patient with the knowledge and skills to manage their anxiety in the long term, promoting independence and well-being.
Remember: This is just a sample example, and the specific approach will vary depending on the individual and their unique situation. Collaboration between the patient, therapist/counselor, and support system is crucial for success.
In our blog we cover issues related to modern healthcare systems and their challenges: doctor-patient communication, digital healthcare services, data security, as well as reviews on popular software for healthcare professionals.
Here's a selection just for you:


