Today’s healthcare professionals want to do right by their patients. Sometimes that means thinking about how we improve business processes and using the best tools for the job.
Telemedicine (also called telehealth) is an emerging practice in healthcare that comes with clear benefits. But like all technologies, there are easy ways to misuse it — and in the world of healthcare, that can have serious consequences.
Just as with standard healthcare, there are circumstances where telemedicine medical malpractice can occur. It is just as important for any professional involved in telemedicine to be aware of what issues they may face and to ensure that they provide a reasonable standard of care to all their patients. In this article, we’ll explain the basics of telemedicine and how best to avoid its common pitfalls.
Learn how to simplify your practice workflow and free up more time for patients with Medesk.
Open the detailed description >>Understanding Telemedicine
To avoid telemedicine malpractice, we need a solid understanding of the technology. Luckily, telemedicine as a concept is very easy to grasp.
It’s likely that you’ve already started using new technology like practice management software to help things run more smoothly. From that perspective, telemedicine isn’t too big an adjustment.
Telemedicine, or telehealth, is when we deliver healthcare to a patient remotely. A doctor might speak to a patient over the phone rather than in person, for example, or send them crucial information via a text message. Such modern technology can still use the reassuring features of traditional telephony, such as local area codes. Customers in California, for example, will recognize area code 747 when you contact them.
Naturally, today’s healthcare professionals can also use more sophisticated technology. It includes tech-like and video conferencing tools to speak to a patient more effectively. Other hi-tech examples of telemedicine include cloud storage of patient files or monitoring a patient’s medical device from a great distance.
Telemedicine has increased tremendously in popularity over the last few years, alongside other practices that benefit from the underlying technologies. It's especially valuable in the context of healthcare. This is because the people who use it may have limited mobility or live in remote parts of the country.
Medesk helps automate scheduling and record-keeping, allowing you to recreate an individual approach to each patient, providing them with maximum attention.
Learn more >>Telemedicine helps patients and medical professionals to bridge this gap and ensures more people receive the healthcare they deserve.
What is malpractice?
Medical malpractice, whether in standard healthcare or telemedicine, happens when the professional providing care makes a mistake or neglects something in the care they offer.
Medical malpractice occurs when a healthcare professional neglects to provide appropriate treatment, take appropriate action, or give substandard treatment that causes harm, injury, or death to a person. Between 1990 and 2020, there was an average of around 47,000 medical malpractice suits every year.
Charges of malpractice can be leveled against anyone providing care, from primary physicians to ED doctors to social workers to midwives. The effects of malpractice can be wide-ranging and can include minor issues, permanent disability, and even death. Settlements in malpractice cases can also be costly; in 2023, a jury awarded a settlement of $180 million to a child born with severe brain injuries as a result of malpractice.
As malpractice can cover any substandard care that leads to injuries or death, then the areas where errors can be made involve every step in the care pathway. Some of the most common malpractice errors happen in these areas:
- Misdiagnosis. When a health professional fails to diagnose an illness—or diagnoses incorrectly—then they may be sued for malpractice. This is something that can happen with telehealth.
- Surgery. Although this doesn’t occur within the telemedicine field, surgical errors are one of the most common forms of malpractice. It can cover everything from operating on the wrong body part to using the wrong equipment (or even leaving something inside the patient).
- Failure to treat. If a healthcare professional either fails to take steps to carry out a diagnosis or if diagnosed, doesn’t treat your condition, then they can be liable for malpractice.
- Birth. This area of malpractice usually involves some sort of injuries to the mother or baby during childbirth which can be anything from bruising to brain damage.
- Prescribing errors. This is an error that anyone practicing telemedicine needs to be very aware of. It can include prescribing the wrong medication, the wrong dosage of a drug, prescribing a drug the patient is allergic to, or even failing to prescribe anything.
Addressing the Risks of Telemedicine
Of course, keeping patients at arm’s length from their healthcare providers in this way inspires some concerns. Some relate to whether people can access telemedicine in the first place (if they have limited internet access, for example). But many more are around the standard of care provided during contact.
As such, healthcare providers risk opening themselves up to accusations of malpractice. To avoid such a scenario, here are some key concerns to think about when you’re communicating with patients in this manner:
#1. Technical challenges
This is one of the most obvious concerns and one of the easier ones to address. While app testing lets us spot problems before a product releases, it’s not always plain sailing. It’s likely that even with a good internet connection, you’ll sometimes have to contend with glitches, dropped video or audio, or even a struggle to connect in the first place.
Healthcare professionals can also encounter issues with other tasks, such as transferring files digitally from one place to another. The files themselves can become corrupted, or the wrong files can be transferred.
More serious issues arise when we have to transcribe medical records. A misinterpreted note can, naturally, have serious medical consequences for a patient. This problem becomes more likely if we outsource the transcription of written messages to people without medical experience. All of these make it more likely a poor level of healthcare is provided, with an increased risk of legal action from your patients.
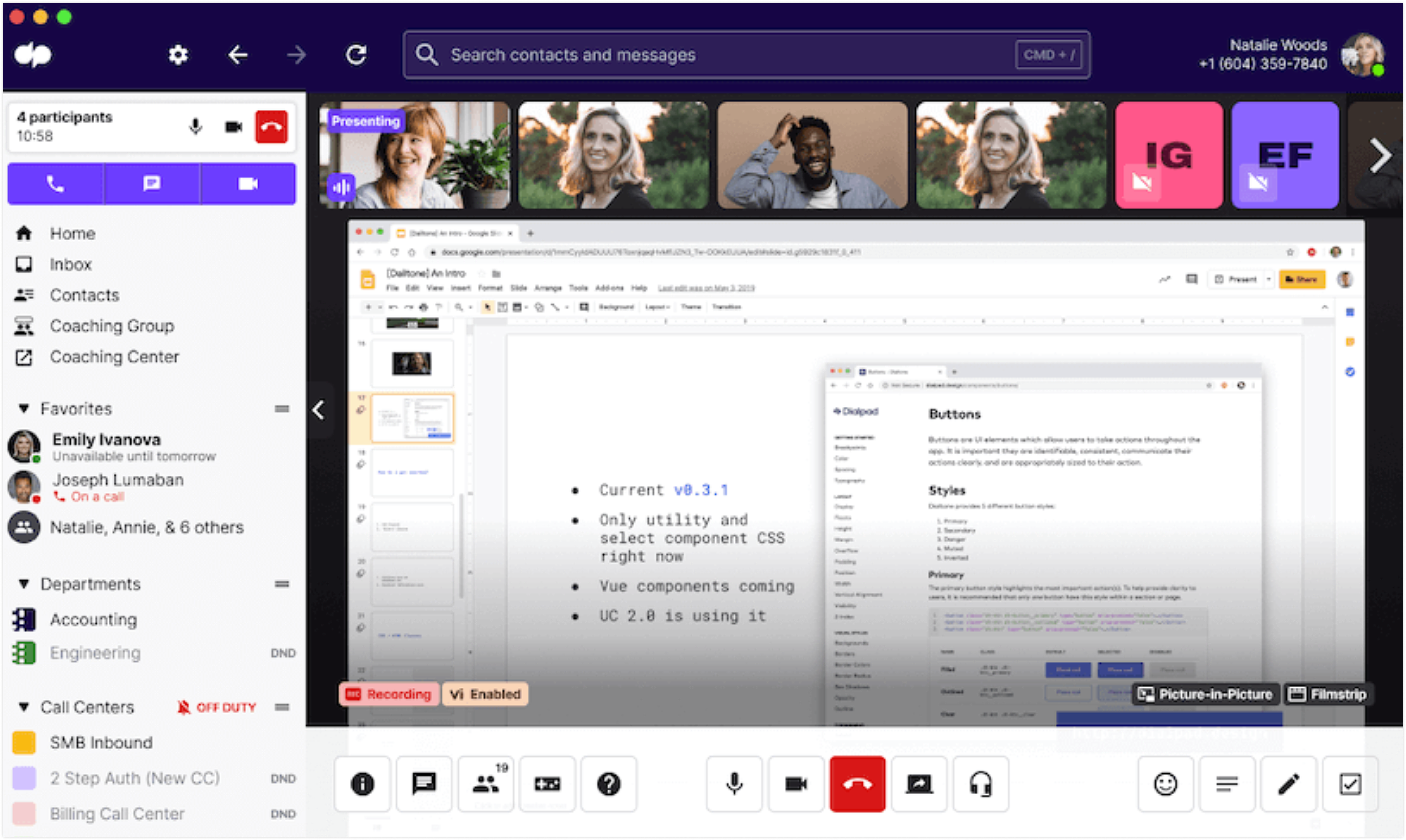
To resolve these issues, think carefully about the specific technology you’re using to provide telemedicine. Look for a video conferencing platform that offers high levels of reliability and security; you don’t want sensitive patient communications to fall into the wrong hands.
If you need to transcribe hand-written notes, ensure the people doing so have a medical background.
Another solid strategy here is to, as much as possible, have another professional with you during conversations. The specific person doesn’t matter much, provided they have a baseline of medical expertise (like a nurse or physician assistant). Virtual team communication tools can help you set this up. One thing that may help in this area is AI audio transcription, which may prove to reduce the occurrence of human error.
Discover more about the essential features of Medesk and claim your free access today!
Explore now >>#2. Diagnosis hurdles
While telemedicine can bridge gaps between doctors and patients, some situations demand in-person contact. Focusing too much on using telemedicine because it’s convenient can mean you miss some signs of illness, something that may leave you open to a charge of malpractice.
For example, doctors may sometimes need to palpate an area of a patient’s body to identify the issue accurately. Lacking these options could compromise a doctor’s ability to diagnose a problem, and virtual meeting best practices (while important) can’t alleviate these issues.
Telemedicine can also present diagnosis problems in branches of medicine where you wouldn’t expect to find them. On the surface, radiology seems like a practice that benefits from telemedicine. This is because much of it revolves around looking at various texts and images, such as X-rays, MRI scans, ultrasounds, etc.
While today’s technology makes accessing these images simple, its ease of use may unwittingly increase the professional’s workload. This may mean they fail to spot crucial signs of illness.
To alleviate this problem, it’s vital to consider if telemedicine is an appropriate choice for each specific situation—especially if a hands-on approach is necessary. When you need to participate in a telemedicine appointment, ensure you keep highly accurate and comprehensive records of what transpired. A voice transcription tool can assist in this kind of task.
#3. Regulations
Even if you can resolve some of the issues with the distance that telemedicine presents, you should check if there are roadblocks around actually prescribing a treatment. For example, the US state of Arizona doesn’t allow pharmacies to distribute drugs using prescriptions given via telemedicine. In-person checkups are also required in this scenario to avoid legal consequences.
It’s also important that you’re licensed to practice medicine in the right areas. US law typically states that clinicians must be licensed in the state where their patient resides rather than where the clinician practices. While this isn’t often an issue with in-person appointments, the rise of telemedicine presents new issues in this area.
It’s also important to consider other relevant legislation, like the Health Insurance Portability and Accountability Act. HIPAA demands that healthcare providers safeguard protected health information (which varying types of data ingestion can help with) that could influence things like your choice of technology.
While we’ve already touched upon this from a call quality perspective, it’s also crucial to consider it from a regulatory one. It’s unlikely that you would use them, but it’s best to avoid the likes of Facebook Live and Twitch in this context.
Ensure that the platform you choose cannot be hacked (or eavesdropped on) to remain in compliance with HIPAA. Register your domain names in the territory in which you operate — purchase domain name Canada, for example, if that’s where your practice is based.
You should also make sure you don’t overlook the issue of informed consent. It’s easy to neglect this principle as a healthcare provider, thanks to the more informal nature of telemedicine.
Address this problem by thoroughly understanding the legalities of practicing and prescribing medicine in your area. There may be lessons you can learn from other industries in how to manage collection of medicines. You may also benefit from brushing up on the concept of informed consent and how to properly apply it in a telemedicine environment. Be aware that the law in this area of medicine may shift rapidly over a short period.
#4. The personal touch
While it’s harder to quantify, it’s important to consider what kind of relationship you’re building with your patients. This is because the better your relationship with them, the lower the chance they will sue you for something you’ve done (or failed to do).
While this might be because you’re offering a better standard of healthcare (and things like online booking) it’s often because things like empathy and compassion are best conveyed when we’re in a face-to-face meeting—and it’s harder to sue someone you care about. This contact allows medical professionals to build a rapport with patients, better understand their problems, and help patients feel that somebody cares about them.
It is possible to have this kind of personal touch during a telemedicine conversation, but it requires a conscious effort and training to carry off properly. As such, this is another reminder that telemedicine is best used as a supplement to conventional patient appointments rather than a replacement for them.
Discover more about the essential features of Medesk and claim your free access today!
Explore now >>Don’t forget to take care of yourself, either. You need to know how to deal with professional burnout to ensure you provide quality healthcare.
The Takeaway
There is little doubt that telehealth offers many benefits, both to patients and to healthcare professionals. However, it is important to note its limitations and the potential for errors to be made. Some things that may be used to give an accurate diagnosis, such as an MRI scan, are impossible to carry out by phone. But when used properly, telemedicine can help overworked professionals and can also benefit patients living in remote or rural areas.
As some of the potential errors that can lead to malpractice are the same in both standard healthcare and telemedicine, it’s essential that professionals try to maintain the same standard of care in both areas. If there is doubt, then a professional healthcare provider should consult with a colleague or a more senior practitioner. There is nothing wrong in admitting you are unsure about something. In fact, it’s quite the opposite and can reflect positively on your professionalism.
One thing you need to consider strongly if you’re practicing telehealth is confidentiality. You need to ensure that you are complying fully with HIPAA regulations and that any communications equipment you use—and how you store patient data—will not allow accidental information leaks or be susceptible to cybercriminals’ attacks.
Take Your Healthcare to the Next Level
Telemedicine is an invaluable tool for healthcare professionals nowadays, as we increasingly use technology to bridge long distances. It can be the perfect way of providing healthcare to people traditionally deprived of it. From that perspective, telemedicine shouldn’t be overlooked by any healthcare provider.
At the same time, it’s integral to recognize telemedicine’s drawbacks—particularly around security and the overall standard of healthcare. It’s essential to work consciously to alleviate these problems and recognize telemedicine isn’t a silver bullet.


