The study of children, especially at an early age, requires a special approach, knowledge of certain techniques used in pediatric practice, skills in behavior and treatment. This is not only with patients, but also with parents experiencing anxiety and concern for their child's health.
The CDC recommends that children have wellness visits at 1, 2, 4, 6, 9, 12, 15, 18 months, 2 years, 2.5 years, and 3 years, and then annually until they reach 21 years of age.
Accurate paediatric history-taking is a cornerstone of successful healthcare delivery for young patients. It forms the foundation upon which clinicians build their understanding of a child's medical history, symptoms, and overall health.
In this article, we will explore essential techniques and best practices that help healthcare professionals optimize care for paediatric patients. This will ensure comprehensive and effective treatment.
Learn how to simplify your practice workflow and free up more time for patients with Medesk.
Open the detailed description >>Conditions for a High-quality Examination
Your image is important. Doctors should be neat: in a clean robe, hair tucked under a cap. It is necessary to minimize cosmetic use. Hands should be clean, warm, with short-cropped nails, washed before examining each child.
Building trust
Paediatric history-taking begins with building a rapport with both the child and their parent or caregiver. Establishing trust and open communication is crucial to eliciting accurate information. Create a comfortable environment, use age-appropriate language, and engage in active listening to put the child and their family at ease.
Before the examination, it is necessary to contact the child, as far as his condition allows. Older children should get to know each other better: find out their names, take an interest in academic success, hobbies, habits.
Use simple language for younger children and gradually adapt to more complex vocabulary for older ones. Ask questions in a non-threatening manner to encourage honest responses.
The doctor should:
- have an even, calm mood
- show patience, self-control
- never get annoyed with the child, his mother and other loved ones.
Involving parents and caregivers
Parents and caregivers play a crucial role in providing important medical and developmental information about the child. Encourage their active participation, ask for insights, and ensure they understand the importance of their input into the diagnostic process.
Prioritizing the chief concerns
Identify the chief concerns early in the history-taking process. Allow the child or caregiver to express their main worries, and then gather information related to those concerns. This helps focus the assessment and prevents essential details from being overlooked.
Сonditions for the premises
During the physical examination of the child you should remember:
- to examine the patient in good light (preferably daytime), placing the child closer to the light source;
- before the age of 3, the child should be stripped naked, and school-age children (especially girls during puberty) should be undressed gradually as the study progresses. However, the child should not be kept undressed for too long because of the risk of hypothermia;
- the room should be warm, 71-77℉ (22-25℃).
The Process of Paediatric History-Taking
Paediatric practice collects anamnesis from relatives, most often from the mother. Nevertheless, it is important to question the child himself, especially if the child is older.
The questioning is the first stage in the child's study and is carried out in 5 main directions:
- Clarification of passport data (name, date of birth).
- Signs of the disease (presenting complaints).
- The past history of the disease’s development.
- The patient's social history, including heredity, birth history and living conditions, etc.
- Epidemiological and drug history (information about contacts with infectious patients).
The collection of disease anamnesis begins with the sign that appears first. In chronological order, you should identify the detailed characteristics of the signs, and how one changes when the other appears. This section should include the results of all previously conducted studies, therapeutic measures and effectiveness. The collection of disease anamnesis is a step-by-step process and is supplemented with additional information as the patient is monitored.
Here are lists of the must-asked questions during examinations of children.
A young child’s history taking (up to 3 years old)
- How did the pregnancy of this child proceed?
- Prenatal regime and nutrition. Was maternity leave used and how?
- How did the birth proceed (duration, complications, mode of delivery)?
- Did the child cry out immediately after birth?
- Birth weight and height.
- Characteristics of the newborn period: assessment on the Apgar scale 1 and 5 minutes after birth, feeding technique (free, by the hour, night feeding, etc.), immunisation in the maternity hospital.
- Borderline conditions of newborns (physiological weight loss and recovery time, jaundice, uric acid infarction, etc.).
- Diseases during the newborn period: rhesus conflict; birth trauma; rashes, septic diseases; wheeze; gastrointestinal diseases, etc.).
- Dynamics of the child's development: holding the head, sitting, walking, mental development.
- Sleep, its features and duration.
- Kind of feeding (natural, artificial, mixed).
An older child’s history taking
- How did he develop at an early age?
- The child's behavior at home and in a team, for schoolchildren - school performance, what subjects does he prefer?
- Past medical conditions and surgical interventions.
- Preventive vaccinations.
- Tuberculin tests, when conducted, their results.
- Sexual development of the child.
Medesk helps automate scheduling and record-keeping, allowing you to recreate an individual approach to each patient, providing them with maximum attention.
Learn more >>Family history
- Surname, first name, profession of parents.
- The state of health of parents and immediate relatives on the mother's and father's side.
- The state of the family tree within three generations, starting from a sick child to grandparents up, i.e. vertically, and up to brothers and sisters - horizontally.
- How many children are in the family, their health.
Social and living conditions
- Where do parents work, their profession, total earnings, the number of family members?
- Characteristics of housing conditions (illumination, heating, temperature, ventilation, dampness, etc.), the number of children and adults living.
- The quality of child care (does the child have a separate bed, how often does he wash, is he provided with linen, does he have clothes for the season, toys, a children's library, does he observe the daily routine, the diet, what is the duration of walks and sleep, etc.).
Epidemiological history
- Ask about possible contacts with sick children, adults at the place of residence (in the family, in the neighborhood) or clarify this information with the district doctor.
A carefully collected anamnesis of life, especially family history, makes it possible to identify a child's predisposition and risk factors for a particular disease. This is often realized at later stages of ontogenesis and even in adults.
Let’s look at the example of a history taking for abdominal pain in a paediatric patient.
Example of History Taking for Abdominal Pain
Patient information
Name: Sarah
Age: 8 years
Gender: Female
Date of Visit: July 20, 2024
Chief complaint
Sarah has presented with abdominal pain for the past 2 days.
History of the present illness
- When did the pain start? (2 days ago)
- Onset: Was the pain sudden or gradual? (Gradual)
- Location: Where is the pain located? (Sarah points to the lower right side of her abdomen)
- Character: How would you describe the pain? (Sarah's mother explains that it is a dull, constant ache)
- Intensity: On a scale of 1 to 10, how intense is the pain? (Sarah rates it as a 6)
- Aggravating Factors: Does anything make the pain worse? (Sarah's mother says that movement and eating seem to worsen the pain)
- Alleviating Factors: Does anything provide relief? (Sarah finds some relief when lying down and resting)
- Timing: Is the pain constant or does it come and go? (Intermittent pain)
- Associated Symptoms: Are there any other symptoms accompanying the pain? (Sarah's mother mentions mild nausea but no vomiting or diarrhea)
Past medical history
- Any previous history of abdominal pain or gastrointestinal issues? (No)
- Has Sarah experienced any surgeries or hospitalizations in the past? (No)
- Are there any known allergies to medications, supplements or food? (No)
Family history
- Is there a family history of gastrointestinal conditions or other relevant medical issues? (No)
Social history
- Does Sarah attend school regularly? (Yes, she is in the third grade)
- Are there any significant recent life events or stressors? (No)
Systems review
- Any recent changes in appetite or dietary habits? (Sarah's mother says she's eating less due to the pain)
- Changes in bowel movements or urinary patterns? (No unusual bowel movements or changes in urination)
- Recent travel or exposure to sick individuals? (No travel history or known exposure to sick individuals)
Developmental milestones
- Is Sarah meeting age-appropriate developmental milestones? (Yes, she is achieving developmental milestones as expected)
Conclusion
Based on the history provided, Sarah, an 8-year-old female, is experiencing abdominal pain localized to the lower right side of her abdomen. The pain is dull, constant, and rates at 6 out of 10. It started gradually two days ago and is aggravated by movement and eating. Sarah feels relief when lying down. There are no significant associated symptoms except mild nausea. Her past medical and family history is unremarkable. Further assessment and physical examination are needed to determine the cause of her abdominal pain and recommend appropriate management.
Practice Management Software for Paediatric History Taking
Practice management software streamlines and enhances paediatric history-taking, improving patient care efficiency and quality. Here are some ways practice management software (PMS) aids in this process.
Discover more about the essential features of Medesk and claim your free access today!
Explore now >>Centralized electronic health records (EHR)
You can store and access electronic health records, including developmental history, immunizations, growth charts, and previous visit notes. Having all relevant information readily available allows healthcare professionals to quickly review past details during history-taking, ensuring continuity of care.
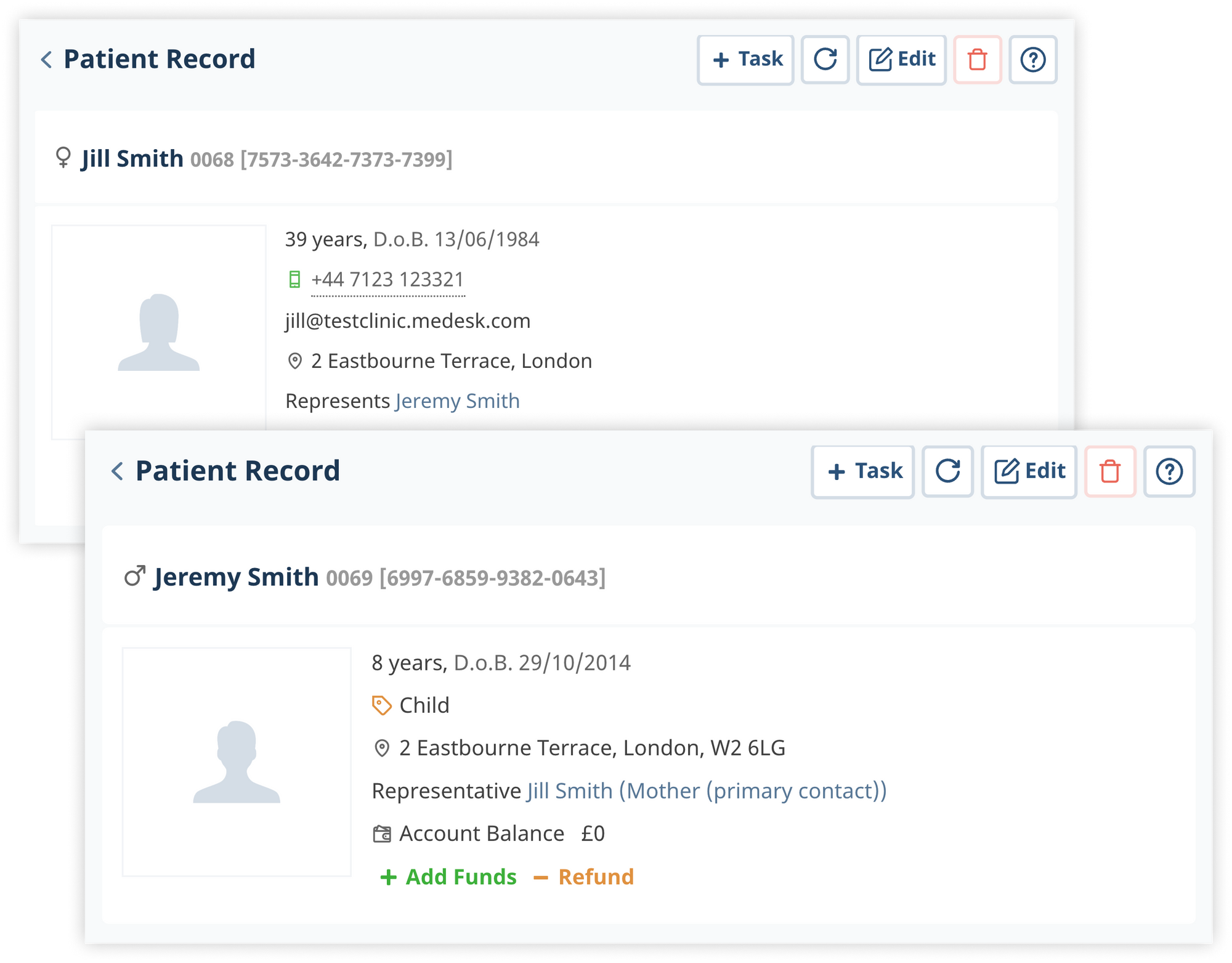
Customizable templates
The software offers pre-built paediatric-specific templates for taking a patient's medical history. These templates prompt clinicians to ask essential questions, reducing overlooking critical details.
Automated questionnaires
PMS can include automated questionnaires that parents or caregivers fill out before appointments.
Alerts and reminders
Set reminders for upcoming visits, vaccinations, and developmental screenings. Additionally, the system can generate alerts for any significant abnormalities or deviations from typical growth patterns.
Telemedicine
In situations where an in-person visit is not possible, practice management software with telemedicine features enables virtual consultations.
Final words
Effective paediatric history taking serves as the foundation for comprehensive and personalized healthcare for young patients.
Unlike adults, children often lack the ability to articulate their symptoms and concerns clearly. This makes it challenging to diagnose accurately through a physical examination. A well-conducted history-taking session allows healthcare professionals to gather crucial information about the child's medical background, developmental milestones, family history, and any recent changes in their health status. It helps clinicians identify potential red flags, early signs of health issues, and possible risk factors, guiding them towards appropriate investigations and interventions.
By implementing practice management software, you atomize note-taking and examination. This allows you to focus on what matters most - providing better healthcare to your young patients.


