The rise of telemedicine during the COVID-19 era has elevated the accessibility of medical services to a whole new level. Today, patients can receive assistance regardless of their location or time zone— all they need is an internet connection.
However, with increased accessibility of medical services comes the need for safeguarding patient data and protection against unauthorized access. That’s where HIPAA, the Health Insurance Portability and Accountability Act, steps in.
In our guide, we delve into essential topics related to HIPAA compliance for healthcare professionals:
- What is HIPAA?
- How do I choose the right telemedicine platform?
- What practices are included in HIPAA compliance?
- What measures are taken for violations?
- How does secure messaging between patient and physician occur?
Stay tuned.
Learn how to simplify your practice workflow and free up more time for patients with Medesk.
Open the detailed description >>Key Aspects of HIPAA: What You Need to Know
HIPAA is a federal law designed to safeguard protected health information. The United States Department of Health and Human Services (HHS) has established a set of rules regulating the confidentiality of patients' medical records. Unauthorized disclosure of private medical information is illegal.
This applies to:
- Healthcare service providers
- Insurance companies
- Information platforms
- Cloud services.
In other words, to all companies and individuals with access to medical information.
During the pandemic, the HHS Office for Civil Rights (OCR) made adjustments to protective measures, making telemedicine more accessible to citizens due to restrictions. When it comes to telemedicine, HIPAA ensures that healthcare providers, referred to as covered entities, and their service providers, known as business associates, adhere to strict guidelines. These guidelines are detailed in the HIPAA Privacy, Security, and Breach Notification Rules.
The HIPAA Privacy Rule establishes national standards for protecting medical records and applies to health plans, clearinghouses, and certain electronic healthcare transactions dealing with PHI.
On the other hand, the HIPAA Security Rule ensures the safety of electronic Protected Health Information (ePHI), which includes any PHI created, stored, transmitted, or received electronically.
Medesk helps automate scheduling and record-keeping, allowing you to recreate an individual approach to each patient, providing them with maximum attention.
Learn more >>Compliance with all these rules and risk minimization can be a costly decision for healthcare professionals. For instance, to use Skype for providing services within the standards, it is necessary to enter into a Business Associate Agreement.
Zoom offers a version of its platform called Zoom for Healthcare that requires the healthcare provider to configure and use the platform correctly. This includes enabling encryption, setting up proper access controls, and signing a BAA with Zoom.
How to Choose a HIPAA-Compliant Telehealth Platform
A platform that securely guards your data should have:
- Secure messaging system
- Data encryption
- Staff training
- BAA (Business associate agreement)
- Integrations
- Security audits
Secure Messaging
Secure messaging pertains to ePHI (electronic Protected Health Information). According to HIPAA guidelines, both covered entities and their business associates must implement measures to protect messages and use various tools for this purpose.
Encryption
Messages containing ePHI must be encrypted to prevent unauthorized access during transmission. Encryption ensures that the data remains secure and unreadable to anyone except the intended recipient.
Access control
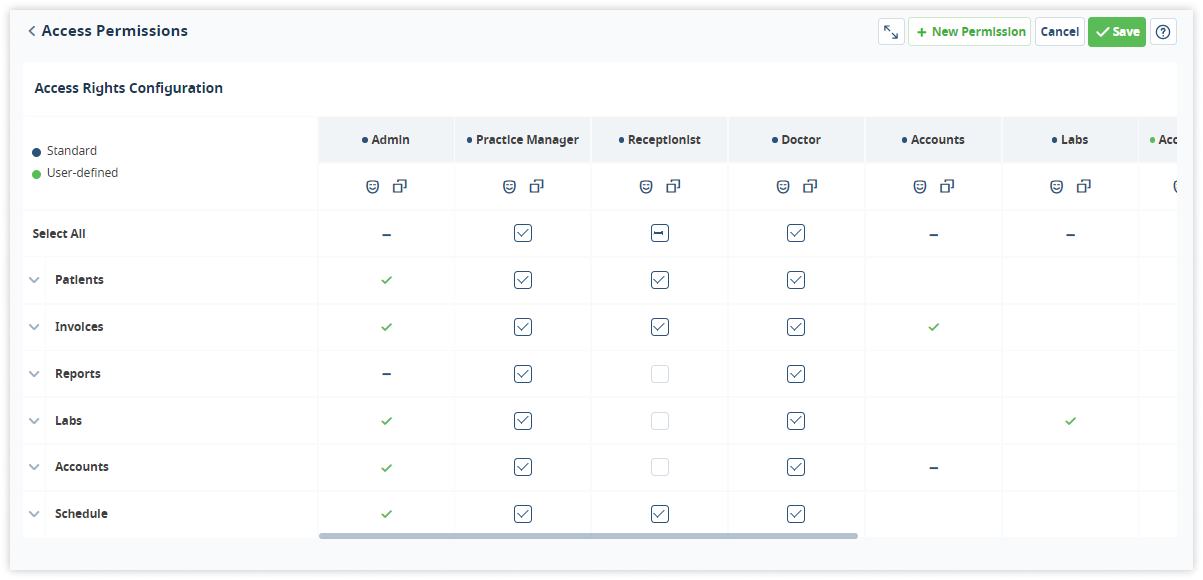
Secure messaging systems should implement access controls, such as usernames and passwords, to verify the identities of users. Access should be limited to authorized individuals, and each user should have a unique identifier to track their activities within the system.
Discover more about the essential features of Medesk and claim your free access today!
Explore now >>Authentication and authorization
Authentication ensures that the sender and receiver of the messages are who they claim to be. Authorization mechanisms define what actions users are allowed to perform within the messaging system, ensuring that only authorized personnel can access ePHI.
Message retention and disposal policies
HIPAA mandates the implementation of retention and disposal policies for electronic messages containing ePHI. Secure messaging systems should have mechanisms to automatically delete messages after a specified retention period to prevent unauthorized access after the information is no longer needed.
Secure file transfer
In healthcare, files such as medical images or documents often need to be shared securely. Secure messaging systems should allow the secure transfer of files, ensuring that attachments containing ePHI are encrypted and protected during transmission.
Secure messaging policies
Organizations should establish clear policies and procedures governing the use of secure messaging systems. These policies should cover topics such as acceptable use, password management, reporting security incidents, and consequences for violating security protocols.
Staff Training
Staff training ensures that every healthcare professional understands his responsibilities and the importance of safeguarding patient information. Here’s how it contributes to security measures.
Understanding the rules
HIPAA rules can be complex, but staff training breaks them down into simple, understandable parts. It teaches employees what they can and cannot do with patient information, ensuring they don’t accidentally breach confidentiality.
Spotting risks
Training helps staff recognize potential risks and vulnerabilities in their daily tasks. By being aware of these risks, employees can take the necessary precautions to prevent breaches.
Password power
One of the basics of HIPAA compliance is having strong passwords. Staff training emphasizes the importance of unique, hard-to-guess passwords. It ensures that employees don’t use easily accessible information, like birthdays, as their passwords.
Email etiquette
Email is a common communication tool, but it can be risky if not used properly. Training educates staff on secure email practices, teaching them how to send patient information safely and avoid accidental disclosures.
Handling electronic devices
In the age of smartphones and tablets, it’s vital to know how to handle electronic devices properly. Staff training provides guidelines on securing these devices, ensuring that patient information isn’t compromised if a device is lost or stolen.
Patient consent
Understanding when and how to obtain patient consent is critical. Staff training clarifies the procedures for getting proper consent before sharing any patient information, ensuring legal compliance.
Discover more about the essential features of Medesk and claim your free access today!
Explore now >>Reporting incidents
Training empowers employees to know what constitutes a security incident and how to report it promptly. Whether it’s a lost file or a suspicious email, staff members should be aware of the reporting procedures to mitigate potential breaches.
Regular refreshers
HIPAA regulations evolve, and technology changes. Regular training sessions keep employees up-to-date with the latest HIPAA requirements and best practices, ensuring ongoing compliance.
Business Associate Agreement
The telehealth services provider should be willing to sign a business associate agreement with covered entities, outlining their responsibilities regarding the protection of patient data. This legal contract ensures that the platform provider shares the responsibility for HIPAA compliance.
Integration capabilities
The platform should be able to integrate with Electronic Health Records (EHR) systems securely. It ensures that medical history is accurately recorded and securely shared between healthcare providers. Seamless integration enhances the overall quality of care you give.

Regular security audits
The platform provider should conduct regular security audits and assessments to identify and address vulnerabilities, ensuring continuous HIPAA compliance and a high level of security.
HIPAA Compliance Penalties
HIPAA compliance penalties play a crucial role in ensuring that healthcare organizations adhere to the regulations. The penalties for non-compliance depend on the severity of the violation and whether the entity knew or should have known about the violation. Here are some examples of HIPAA violations and the corresponding punishments:
Unintentional Violations
- Fine: up to $50,000 per violation, with an annual maximum of $1.5 million.
- Example: accidental disclosure of patient information due to a misaddressed email. If multiple patients' information is disclosed in a single incident, each patient's record may be considered a separate violation.
Reasonable Cause
- Fine: up to $50,000 per violation, with an annual maximum of $1.5 million.
- Example: failure to conduct a thorough risk assessment to identify vulnerabilities in the handling of electronic patient data.
Willful Neglect (Corrected)
- Fine: minimum of $10,000 per violation, with an annual maximum of $1.5 million.
- Example: not having proper technical safeguards in place despite awareness of the risk, but correcting the issue promptly after the violation is discovered.
Willful Neglect (Not Corrected)
- Fine: minimum of $50,000 per violation, with an annual maximum of $1.5 million.
- Example: not addressing a known vulnerability or ignoring a breach in patient privacy, leading to further unauthorized access or disclosure of patient information.
Criminal Violations
- Fine: up to $250,000 and imprisonment for up to 10 years for intentional wrongful disclosure or obtaining patient information under false pretenses.
- Example: deliberate theft or sale of patient records for personal gain.
Individual Penalties
- Fine: individuals who knowingly obtain or disclose PHI without authorization can face fines of $50,000 and imprisonment for up to one year.
- Example: an employee accessing patient records without a valid reason, such as curiosity or personal vendetta.
State Attorney General Enforcement
- Fine: state attorneys general can also bring civil actions against entities for HIPAA violations, resulting in monetary penalties.
- Example: a healthcare organization suffering a data breach and not promptly notifying affected patients, as required by state laws, leading to legal action by the state attorney general.
It's important to note that the penalties can also include corrective action plans, increased oversight by the U.S. Department of Health and Human Services, and reputational damage, which can have long-lasting consequences for healthcare organizations and individuals involved.
Final Thoughts
In the growing realm of telehealth technology, following HIPAA rules isn't just a legal necessity; it's a promise to patient safety. Understanding the rules, picking the right platforms, and using good practices benefits both healthcare providers and patients. Staying aware and taking action is vital to making the most of telemedicine while keeping patient data private and secure.


