According to Statista, the annual number of physical therapists in the United Kingdom has almost doubled from 2010 to 2024. Just look at these numbers:
In 2010 there were about 44 thousand physiotherapists, compared with 78 thousand in 2024
Demand always creates supply, that’s what we are documenting today. Not to mention, Medicare in Australia covers physical therapy sessions.
The more patients, the more overstrained providers’ workflows are. Healthcare providers are trying their best to make the treatment process easier to bear for everyone. That’s one of the main reasons for the growing accessibility and popularity of practice management software and its pre-made templates and questions.
Learn how to simplify your practice workflow and free up more time for patients with Medesk.
Open the detailed description >>Today we are about to discuss a simple but very productive way to lessen the tension during the appointment and to get more time for actual care - writing physical therapy soap notes using an example. You’ll find out:
- Why we need treatment notes in physiotherapy
- What is a progress note
- The benefits of SOAP format
- About Medesk physical therapy template
Let’s get started.
Why Do We Need To Write Physical Therapy Documentation?
Medical information should always be documented, especially when discussing a client’s progress. This simple rule gives a caregiver a range of advantages:
- Trackable health progress
- Structured information
- Urgent details can’t be omitted
- Easy transfer of the case to another specialist.
The process of transfer is very critical, because physiotherapy treatment is prescribed to the patient by the attending physician. And so, in a medical history, a note is made about the prescribed type of physiotherapy and the area of exposure.
It is critical to keep notes because a physiotherapist studies the patient's medical history, assesses the patient at the beginning of the treatment, and prescribes the method of exposure. In a medical history, he notes what physiotherapy treatment is prescribed for, the area of exposure, the type of therapy, and the number of procedures of physiotherapy.
Also, in a physical therapy progress note a professional writes down the tolerability of physiotherapy treatment, the number of procedures taken and their effectiveness. In the discharge summary, the attending physician evaluates the effectiveness of physiotherapy treatment and makes recommendations for further rehabilitation in outpatient conditions.
Medesk helps automate scheduling and record-keeping, allowing you to recreate an individual approach to each patient, providing them with maximum attention.
Learn more >>When writing SOAP notes, it is crucial to include patient admission details to ensure that other healthcare professionals can easily interpret their medical records. This includes briefly explaining who performed each action, what equipment was used, and how each action was measured. It is important to provide evidence for each statement and carefully review the notes to ensure clarity and logical coherence.
Progress Note: What Is It?
A physical therapy progress note is a legal document written by a professional occupational therapist. The aim of a note is to track a patient’s care process, write prescriptions, document complaints, and outline treatment plans.
Clinicians employ the instrument of note-taking to get the most out of the planning process. Every note includes a section called Plan that can be used to modify the treatment if needed. A therapist uses the planning section of a note to make these alternations without interrupting the actual manipulations.
According to Medicare, a progress report must provide an update on the patient's condition every 5-10 visits. An important thing to remember is that a progress note is not an independent part of a medical record. All medical documents are connected with each other, but the information in them must not be reproduced. The plan of care, visit notes, test results, and progress all work together to produce the best functional results.
Discover more about the essential features of Medesk and claim your free access today!
Explore now >>The most widespread format of note-taking in physical therapy is a SOAP format. Let’s consider it in detail.
The Benefits of SOAP Format
While there are many ways a physical therapist can document patient progress, physical therapy SOAP notes are the most comprehensive and structured way to go. These notes are carefully kept in a patient’s medical history providing a detailed picture of his progress, regression, interventions provided and visits performed.
Developed by a physician and researcher, Dr. Lawrence Weed, the SOAP method makes it possible to prepare patient records with a clear goal in mind: well-being, recovery. Physical therapists use SOAP notes to describe in detail their interactions with patients and collect data on their success in physical therapy.
You can read about implementing this type of note in mental health practice here
SOAP acronym represents four key sections of patient documentation:
subjective, objective, assessment, plan. We’ll analyse the components of a SOAP note in detail.
Subjective section
The SOAP notes subjective part of notes summarizes the patient's perception of their condition, care and progress. A patient's description of their experience can provide useful information for medical professionals when making a diagnosis or tracking changes in their symptoms. The information during the physical therapy assessment may include:
- Pain level
- Mood
- When did the symptoms appear or worsen
- Activity level
- Possible environmental factors.
The subjective section highlights how the patient's condition affects them. Physical therapists use the details in this section to document how physical therapy treatments change their overall quality of life. They can use subjective information to adjust the care plan to support patients' morale and meet their overall needs.
The subjective section also offers an opportunity to inquire about the patient's goals. By understanding their aspirations and desired outcomes, we can tailor the treatment plan to their specific needs.
While maintaining the organization and clarity of the SOAP note, it is equally important to include the patient's feelings about treatment progress, changes in function level, evolving quality of life, and their plans to overcome their condition. By incorporating these elements, you can create a thorough and holistic subjective section, promoting effective communication and enhancing patient care.
Objective section
Objective information describes the actions and measurements related to patient care. In this section, physiotherapists describe the methods they use to collect factual information about the patient, and the results of their methods. Listing objective details makes it easier for the physiotherapist to determine progress in physiotherapy procedures. Here are some examples of data that should be recorded in the goals for physiotherapy section:
- Vital signs
- Physiotherapy activities
- Duration of treatment
- Types of equipment
- Range of motion
- Power level
- Ability to balance
- Motor skills tests
- Flexion tests.
For example, if a patient has rheumatoid arthritis, the results of ultraphonophoresis, laser therapy, therapeutic exercises and peloidotherapy should be indicated in this section. Physioprophylaxis and different types of baths have been used to treat systemic scleroderma.
Assessment section
In this section, physiotherapists review the patient's condition and share their professional opinion on the patient's recovery status. Physical therapists can refer to past SOAP notes and identify changes to develop their assessment. This section combines and analyzes information from the first two sections to make predictions about the patient's recovery and assess the success of his current treatment plan. In the assessment section you can include:
- Brief description of symptoms
- Complications
- Interaction with other medical professionals
- Assessment of patient behavior
- Explanation of changes in physical abilities
- Forecasts of future progress
Plan section
In the SOAP plan section the physiotherapist describes the proposed treatment for future physiotherapy sessions. The physiotherapist explains to the patient the methods of treatment at home, referrals to other specialists, prescribed medications and plans for the next personal appointment. Describing their plan, physiotherapists point out each element of treatment and explain any changes compared to previous plans.
So what should you include in this section?
First, you note down the exercises you did during the session and why you did them. Then, write about how the patient responded to these exercises and any improvements you saw. You also mention what you plan to do next and when the patient should come back to see you.
You must make sure to ask the patient about his plans until the next session to give him good care. If the patient's goals change, you update them in this section too.
To cut it short, the idea is the following:
A clear benefit of splitting notes into sections is a convenient workflow during treatment.
What does it mean?
Writing notes makes it easier to follow all stages of the patient journey in your clinic: scheduling, examination itself, billing and patient satisfaction
The length of a SOAP note can change based on different things like how the client is doing, how complicated the session is, and what your practice or organization needs. There isn't a set length for a SOAP note, but it's usually best to keep it short and focused while still including all the important details.
Usually, a SOAP note is a few paragraphs to a page or two long, but it's more important to make sure it's complete and accurate than to stick to a specific length.
Writing Physical Therapy Progress Notes Can Be A Simple Process!
Follow these steps to compose detailed and effective SOAP notes for physical therapy:
#1. Take personal notes
When treating patients, use shorthand to make personal notes about your interactions and observations. Since SOAP notes are detailed summaries of the appointment of a physical therapist, they require focus and dedication.
#2. Determine the goals of treatment
After the physical therapy session, start your notes by writing down your goals for the patient. Goals provide useful context for notes and allow you to quickly assess patient progress. Use specific numbers to describe success rates of treatment, such as walking 100 feet unaided or lifting 15 pounds.
#3. Use a narrative format
When filling out the main sections of a note, use a descriptive format to describe your findings. Tell a chronological story explaining the patient's experiences and what happens during the appointment. The narrative format helps to link each note to a comprehensive story about the patient's recovery through occupational therapy.
#4. Focus on the facts
Be honest when describing your observations. Keep a neutral tone to avoid making assumptions about the patient or passing judgments about actions, attitudes, or progress in treatment. Focusing on the facts of the situation in your notes preserves their integrity as a medical document and allows the care team to make logical choices.
#5. Use precise language
Include patient admission details so that other healthcare professionals can easily interpret their medical records. Briefly explain who performed each action, what equipment they used, and how you measured each action. Provide evidence for each statement and review them carefully to make sure the notes are clear and logical. Clarify any vague wording and organize your thoughts to make it easier for the reader to understand.
#6. Prepare notes
After filling out the SOAP note, add it to the patient file. Write down the date of the meeting and organize the notes in chronological order. They are most useful when you can easily access them to find out how a patient's physical abilities change in response to different types of treatment.
If you work with your patients remotely, you still need to take notes. But you have the significant advantage of switching from paper to electronic health records. Digital notes are easy to access and fill in due to the built-in progress note templates.
#7. Prioritise key information
Determine the key data required for documentation in every segment of the SOAP note. By prioritizing essential details, you will streamline the process, and minimize time spent on less crucial information.
#8. Use abbreviations
Abbreviations and standard phrases are really important when writing objective SOAP notes because they make things faster, more accurate, and save time. When you create a list of common short forms and phrases that you use a lot in a specific area of healthcare, it helps you quickly write down the same information in SOAP notes.
Plus, using the same phrases every time makes sure your notes are consistent, clear, and easy to understand by other healthcare workers.
Digital Physical Therapy Template
If you want to make progress note-taking a time-saving process, you should take a closer look at practice management software with the function of electronic health records and pre-made physical therapy assessment templates.
The advantages are too numerous to ignore:
- ICD-10 databases
- Uploading documents to medical history
- All plans and notes in one place, so the data is safe
- Function of automatically data adding
- Variety of forms and templates.
With an EHR system, you can devote yourself to the patient instead of being distracted by endless paperwork.
Previously completed consultation notes are a real magic wand.
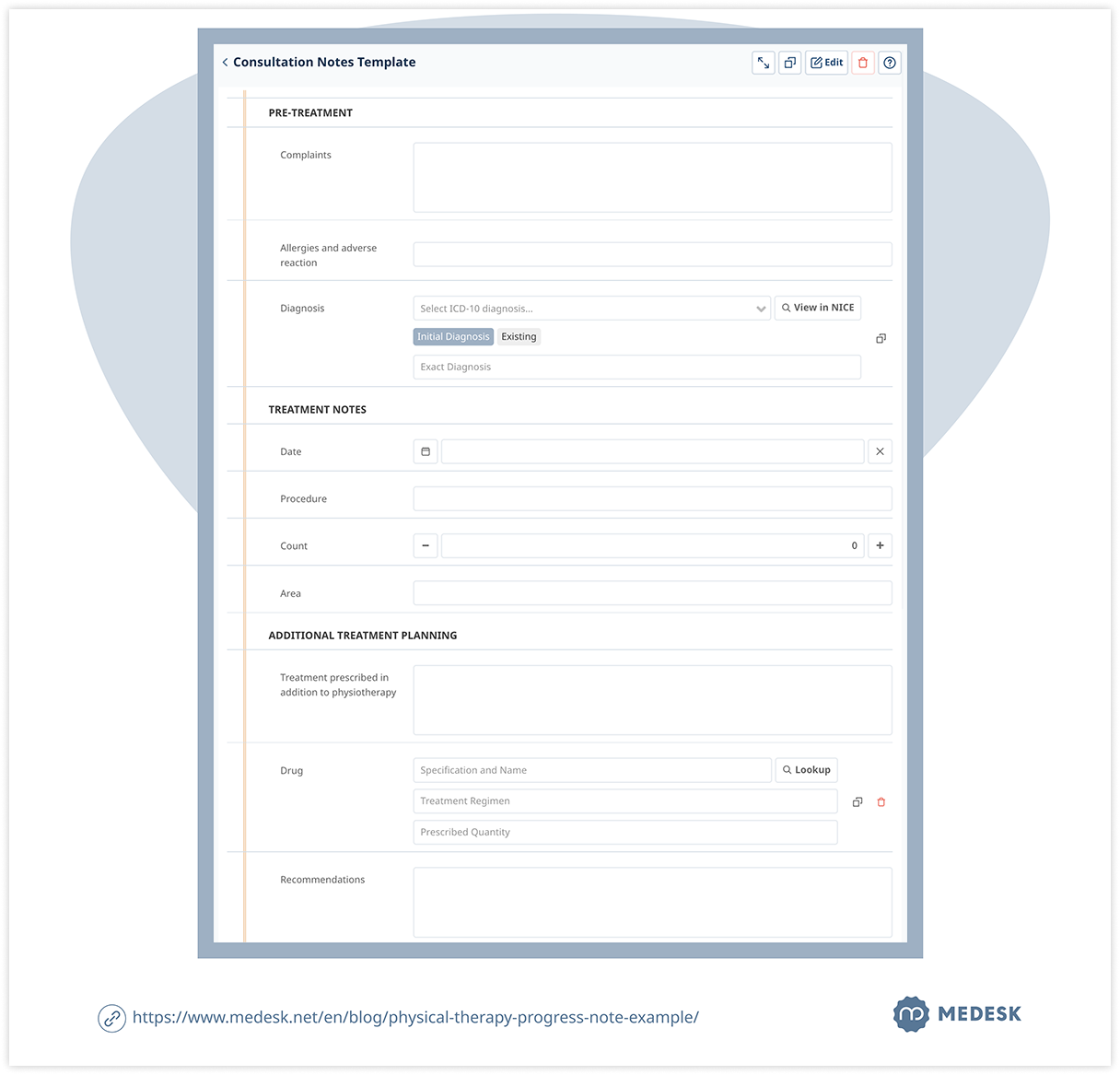
For your convenience, the note is split into 3 sections:
- Pre-treatment
- Treatment
- Additional treatment planning.
By filling in all the sections (which is very quick due to the pop-up options), you’ll have a comprehensive progress note within minutes.
Taking notes as you go during a session or test is really helpful. It means you can write down important stuff while it's still fresh in your head. This way, you're less likely to forget anything important later.
So, it's really important to take notes as you go with EHR and PMS because it ensures that you have reliable info that's easy to access, and it lowers the chances of missing anything crucial.
Don’t forget that a clinician who doesn’t take his eyes off his papers is less likely to impress a patient, leaving you unsatisfied. By using a PMS, you can minimise errors and strengthen patients' trust.


